Dual Diagnosis Treatment
What Is Dual Diagnosis?
A dual diagnosis is when a person is diagnosed with having both a psychiatric condition and a substance use disorder at the same time. Another scientific term used to refer to this condition is “co-occurring disorders” (COD). There is no distinction made for which condition appeared first or whether one caused the other. The concept of dual diagnosis is not a new one as the term has been around since the 1980s. However, it is only in recent years that the medical community has recognized that this complex condition requires a unique drug addiction treatment approach.
What makes dual diagnosis so particularly challenging to treat is comorbidity, a circumstance where the interactions of two simultaneously occurring condition can influence and worsen the other. Often, comorbidity occurs in an ongoing cycle that’s so interwoven it can be difficult or even impossible to attribute the symptoms of either condition or another. This in turn makes it identify and treat the true root cause of the issue.
There is a sizeable overlap in the way in both addiction and mental illness affect the brain. Many of the same mechanisms that cause addiction can cause or exacerbate mental health disorders, and vice versa. Whether the mental illness is pre-existing or not, its presence can make individuals more prone to turning to drug use in the first place, and much more likely to develop addictions. The behavioral side effects of either condition also contribute to the actions and mindset that increase an individual to develop a substance use disorder. As such, the complex nature of co-occurring disorders has unique treatment needs that makes traditional addiction treatment approach of cognitive behavioral therapy (CBT), far less effective.
For these reasons, it’s vital that any addicted person who has a form of mental illness, serious or mild, enrolls at an addiction facility that is capable of addressing both conditions simultaneously. Dual diagnosis treatment centers specialize in addiction rehab that specifically targets both addition and mental illness through specialized types of therapy and uniquely tailored curriculum. These programs recognize the complex relationship of the two disorders and offer a different approach to that of standard addiction treatment.
The Connection Between Mental Illness & Addiction
Most psychiatric conditions are caused by a neurochemical deficiency—something that can both be caused or worsened by substance abuse. Although the exact reasons why mental illness and addiction coincide so frequently are not yet fully known, research has confirmed that dual diagnosis patients often have a higher proclivity to turning to substance abuse and developing a physical dependency. Once dependency has taken hold, it often results in more deeply-rooted addictions compared to those without mental illness, and ones that can be extra challenging to undo.
In many cases, people suffering from mental disorders try to self-medicate by turning to substance abuse as a way to cope with their struggle—particularly those with an undiagnosed mental illness. It has also been proven that consumption of alcohol or drugs at an early age can trigger the development of mental disorders. It’s virtually impossible to determine which came first: the mental disorder or addiction. In addiction treatment, it does not matter as the only concern is providing a specialized program that can target both conditions at once.
Common Dual Diagnosis Pairings
As awareness of the connectedness of mental illness and substance abuse has grown, research has found that even mild mental illness, can heighten a person’s risk with addiction. Below are some of the most common dual diagnosis pairings:
Dual Diagnosis Statistics: Who Does It Affect?
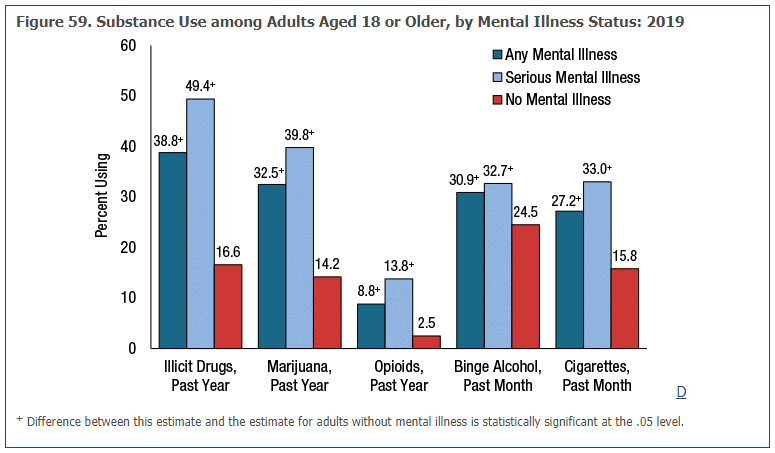
According to the most recent data from the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2019 it was reported that 9.5 million Americans have both a substance abuse and a mental health disorder (approximately 3.8% of the total population). However, these numbers are likely much higher as more than half of all adults and children with a mental health condition don’t receive treatment or are properly diagnosed. Those 18 and older who have a mental illness have been found to up to 3 times more likely to use illicit drugs and marijuana, twice as likely to smoke cigarettes, about 50% more likely to binge drink, and an astounding 5.2 times more likely to abuse opioids.
When it comes to treating co-occurring conditions, the situation is just as bleak. Of the millions of adults with both a mental illness and substance abuse disorder:
- 52.5% never received treatment for either disorder
- 34.5% received mental health care only
- 9.1% received for both conditions
- 3.9% received substance abuse treatment only
Failing to receive dual diagnosis treatment can be dangerous, as an approximated that 1 out of every 8th E.R visit was related to co-occurring disorders.
Maryland Dual Diagnosis Treatment Statistics
In 2013, nearly 40% of admissions for addiction treatment was a dual diagnosis. More recent data from the Maryland Department of Health reported an increase to 45% of adults treated by the state’s Mental Health Authority. In children, this number is smaller but still quite concerning, as 7.4% of those aged 18 or under had a dual diagnosis, which is higher than the national average of 6.2%.
Interestingly, the frequency of co-occurring disorders in Maryland varied depending on the type of drug. Benzodiazepines (benzos), were the drug most likely to be associated with a coexisting mental illness and addiction. Heroin and alcohol, however, experienced the greatest increase in abuse rates by Maryland residents with a mental illness.
Symptoms & Signs of Dual Diagnosis
The symptoms one might manifest when diagnosed with two different disorders can be as diverse as the many combinations that can make up a dual-diagnosis case. It’s true that mental disorders and addictions have their own characteristics. But, there are some signs and symptoms that are common to multiple illnesses. People who are dealing with co-occurring disorders might experience:
- Excessive use of alcohol and/or drugs and overdoing it both in dosage and frequency
- Not being able to keep up with their usual schedule and routine at work or school
- Failure to complete common daily tasks, like taking care of personal hygiene
- Changes in their social circles and places they usually go to
- Putting themselves in risky situations for no specific reason, impulsively or not
- Frequently avoiding people and events that they once enjoyed
- Uncomfortable withdrawal symptoms whenever not consuming drugs (and that might worsen their mental disorder symptoms)
- Experiencing changes in thought process, either becoming incoherent, disillusioned, and/or expressing dark and suicidal thoughts
- Sensory hallucinations, either caused by drug consumption or by mental disorders
- Having a family history of psychiatric disorders and/or substance abuse
- Showing difficulty accepting the idea that they need treatment or following through with it once it’s started
One of the reasons why dual-diagnosis disorders are hard to diagnose and treat is because many symptoms of withdrawal are also symptoms of mental disorders, such as anxiety and depression. That is another reason why it is so hard to tell which disorder occurred first, too. Overlapping symptoms are a problem when deciding on how to approach each disorder and how to medicate and treat a patient.
Experts have said that an early diagnosis of a mental health condition can lower the chances of the development of a substance use disorder. Treatment in the early stages can cut the risk of substance abuse during the teenage years. And the same goes for substance abuse: early treatment of addiction can help prevent the onset or improve the outcome of mental illnesses that can be triggered by it.
What Is The Dual Diagnosis Treatment Process?
There are treatments available for both addiction and mental disorders in general. So, it is possible to treat someone suffering from co-occurring disorders. However, a dual-diagnosis treatment program will not be the same as a single-diagnosis one. There are many different ways to approach co-occurring disorders.
A person who is suffering from two disorders needs to treat each disorder accordingly. It can be done sequentially (treat the most acute disorder first and the second one later). It can also be done at the same time. But they each require a different approach, separate tracking of improvement, and need to be addressed separately.
Usually, the first step in the addiction treatment process is detoxification. It works to flush all the toxins from the body in order to start the treatment fresh. Once this initial stage is over, a patient will then start treatment for their disorders. All programs include both medical and psychiatric procedures in order to treat symptoms, help the system start going back to normal, fix any major chemical and neurological imbalances, etc.
Another important part of the process is therapy sessions, both in individual and group settings. These sessions are a useful tool, and it is recommended that patients continue sessions even after their treatment, whether by going to the same groups or trying new ones. The patient can address their issues during these sessions. They will also have an opportunity to start new relationships and feel less alone in their journey, understanding themselves through others.
Types of Dual Diagnosis Treatment Options
When choosing the right program, the options available tend to fall under two possible categories: inpatient treatment and outpatient treatment. The main difference between the two is that the former requires a 24-hour stay in the facilities, while the latter lets the patient stay home and only come to the facilities for sessions of treatment. The duration of each depends on the patient’s condition. Inpatient programs last at least a month or so. Outpatient rehab programs might take longer since treatment is not continuous.
For outpatient programs, there are different service settings to pick from. A partial hospitalization program, for instance, is almost as intense as an inpatient program. It requires up to 5 to 6 visits a week. Another more moderate option is the intensive outpatient program. Visits are less frequent and don’t last as long ‒ only a few hours a day. As a “rule of thumb”, the milder the symptoms, the fewer visits are required (although only a practitioner can say how frequent they should be).
Get Help Right Now at The Freedom Center
If you or a loved one suffer the afflictions of dual diagnosis in Maryland or any other state, we at The Freedom Center can help. Our dual diagnosis treatment center offers specialized programs with personalized plans that help you address both disorders and transition into sobriety at your own pace.
Our dual diagnosis treatment programs offer everything from the basics, such as therapy and medical help, to holistic treatment and even legal aid – everything to make your life easier as you receive treatment. We are dedicated to helping our clients overcome and stay free from addiction.
Visit our website to learn more about our programs and our values and contact us today. Our team will be happy to answer your questions as you enter this new lifelong journey to reach the best version of yourself. So, call us at (888) 530-5023 to find out how we can help you!